Does scar tissue from a core muscle repair change breathing mechanics?
I’m re-reading Jill MIller’s “Body By Breath” and am trying to apply some of the concepts in her book - which is a bloody tome by the way. As part of it, she proposes that your breathing mechanics, respiration, and resting tone of the supporting structures all have interconnected affects on the body’s state of parasympathetic vs. sympathetic tone.
This is nothing new to Yogis, swimmers, and other people who are keen on breathing. Nor is it to me. But as part of that, the intellectualized understanding of a concept is very different from a visceral understanding of a concept; this is especially true once you start layering in structural changes to the systems (like two abdominal surgeries in my case)
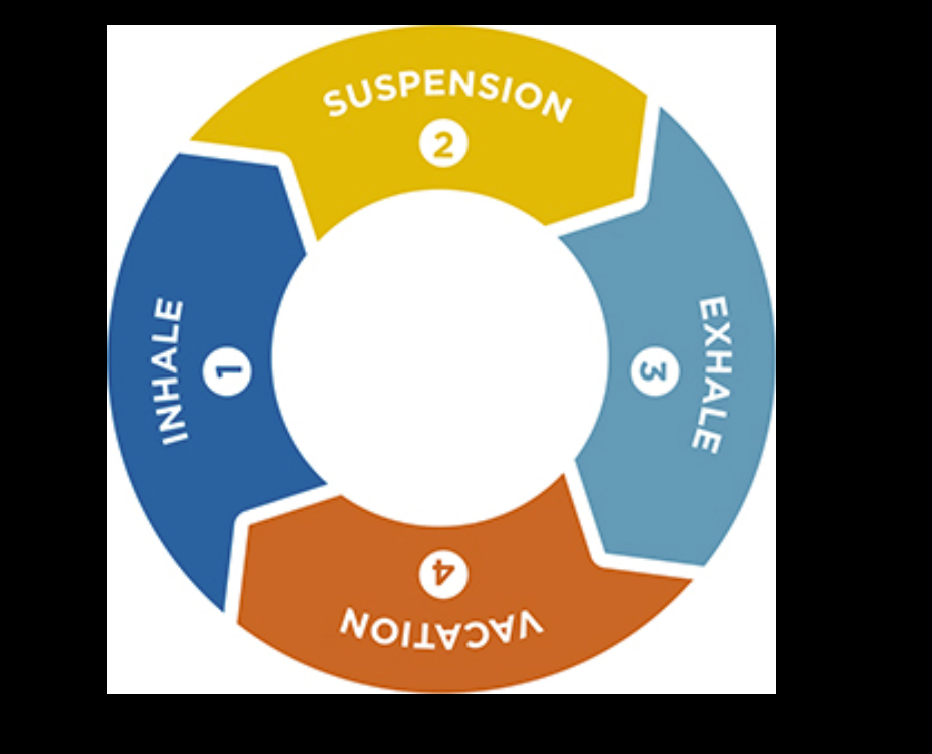
Let me illustrate. Jill aptly shows that there are really only four parts of a breath cycle.
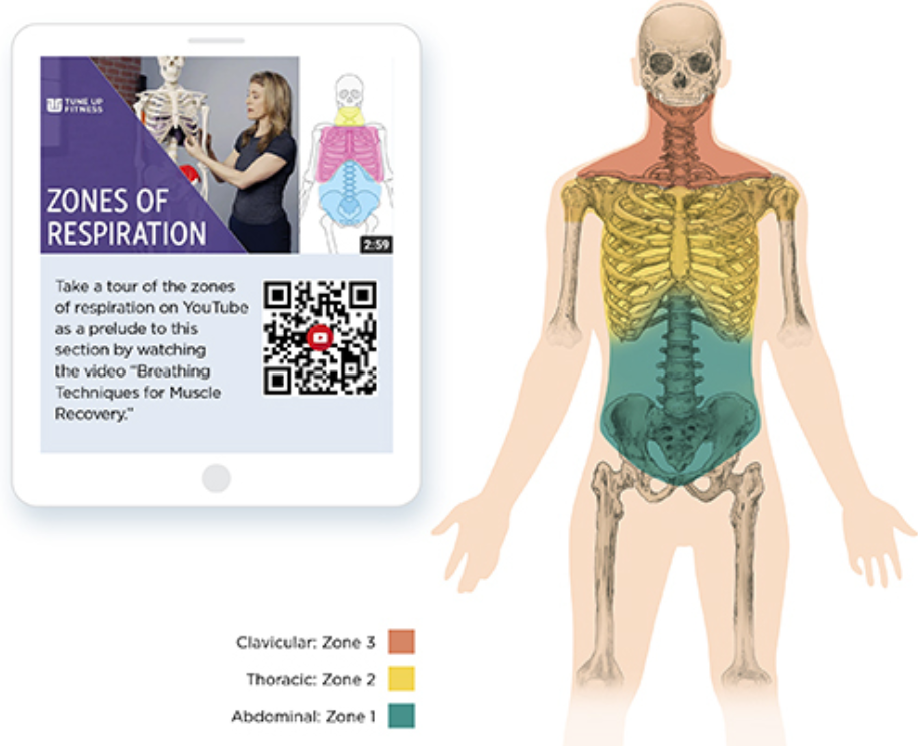
Inhale. Hold at the top. Exhale. Hold at the bottom. Every breath is composed of some variation of this sequence. Making matters even simpler, there are also only three zones of respiration: abdominal, thoracic, and clavicular.
I'll skip some of the details here (so you'll buy her awesome book) but these different zones serve different respiratory purposes as well as having different affects on your state of para-sympathetic / sympathetic balance. The concepts are rather straightforward but complex in practice.
We could talk about athletics, dance, sex, daily living, meetings, the list goes on. But before any of us talk about the complex stuff I'll aim to start with the basics. How do we breath best for our daily lives as a sedentary population? We have to do it thousands of times a day, mostly under low demands if you're an unfortunately deskbound monkey like me.
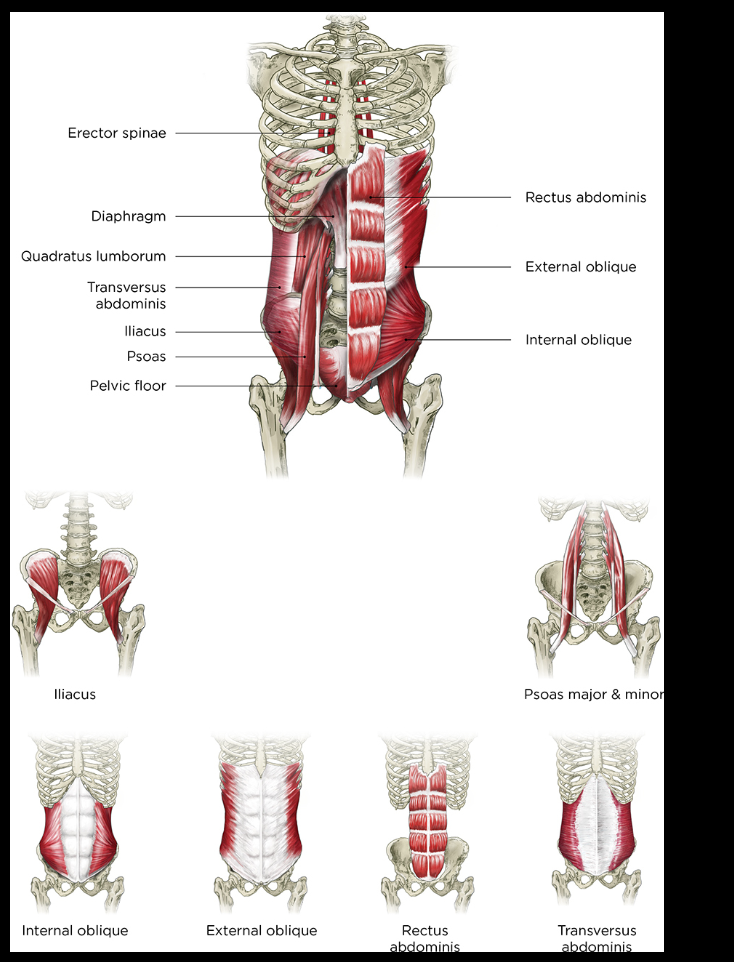
According to Jill Miller, "No other breathing muscles have the longevity for breathing like the diaphragm does. Relying on your breathing synergist muscles creates overuse syndromes and pain. This pain can be local to the breathing muscle, or it can happen in remote areas of the body due to the interconnectviity of your fascia (Miller, location 1977 kindle)."
Let's dig into that for a moment. The 1st argument is that your diaphram is designed for endurance. The 2nd is that using your synergist (helpers)as the primary breathers can actually cause discomfort or pain.
If you're breathing with your zone one respirators, you're using, "Actively, the diaphragm. Passively the transvers abdominis, the internal and external obliques, rectus abdominis, quadratus lumborum, psoas, pelvis floor, and the fascial links between those muscle are mobilized due to the diaphragm's motion. (Miller, location 2021)." If one is breathing this way, it is the, "most sedating and calming of all breathing style and triggers parasympathetic dominance (Miller, location 2021)."
Bingo! That's what we want, right? To be calm throughout the day unless we need to put zone 2 and zone 3 in place that match the as needed demand for extra oxygen delivery. If you've every been to the Slipper Room in New York you will know that the aeriel silk performers are using just about every breath zone available to their body to perform their magic. I was there recently and saw a performer hold a middle splits 25 feet in the air . Though I was mesmerized by the magestical movement, she was breathing heavily using all three zones.
But what happens if you take away someone's ability to breath into zone 1? Does that increase their reliance on zone 2 and zone 3?
Well, should we do so we should get an increase in baseline sympathetic balance, increased tension in the accessory breathing muscles, and a cascading series of downstream affects of increased sympathetic activity based on your specific physiology of the person. For me, it’s dandruff, skin changes, pain, irritation, and an inability to sleep.
I thought this was the case as to why I could never get out of pain. It turned out that I had duel femoral antecebular impingement requiring surgery (see my recovery guide). As of today’s writing, I’m ten days post-op but have not resolved the neck issue.
Now I wouldn’t expect a surgery to be a magical pain cure but it does beg the question - at what point does the unresolved neck pain and middle back pain go away? Was the impingement a cause of the pain or one-of-the-causes in a series of causes?
This is the basis of my abdominal scaring question. As of writing this, I am sitting in a coffee shop on a tall-chair with about a 3/10 pain in my neck, 2/10 pain in my glutes, and generalized tightness in my thoracic spine. Now I’m not going to try to be overly specific in my description of the muscles involved but the hypothesis is that I have adhesions in my abdomen that are changing my breathing mechanics. This is also probably related to a decrease in sensation in my abdominal wall post surgery.
Here is what I have -
An inguinal hernia repair done in 2018
A core muscle injury repair completed in 2020
There is scar tissue laid down in pelvis with two bi-lateral incisions (that look like a separated V) roughly three inches above my pubic symphysis. Two inches laterally to my v-scars on the left side is some remaining scar tissue from the hernia repair.
Put differently, a whole bunch of disorganized scar tissue right in the center of my zone 1 breathing muscles laid over (and possibly within) the pubic symphysis side of my rectus. In addition to this, my core muscle repair surgeon described “significant calcification” of my rectus abdominus. So, does A tight rectus plus scar tissue mean that zone 1 breathing can be restricted? If so, could this leave me in a permanently sympathetic state?
Maybe, not sure really. Though it’s a working theory. To answer that, I go to Fascia, Function, and Medical Applications Chapter 18: Scar Tissue Management (link). Right out of the gate, “It is estimated that 93% of abdominal surgeries result in abdominal adhesions (pp. 234).”
The degree to which these adhesions change my diaphram’’s ability to plunge and does it restrict me to zone 2 and zone three breathing. If it does, what can be done about it?
That answer is still unclear, but the questions are now clearer:
1. Is my abdominal scar tissue changing my breathing mechanics?
2. If so, what can be done about it?
Tomorrow I’m going to ask my physical therapist about this and see what she suggests. If this theory holds water, I’ll then move onto the question of what to do about it and write a separate article.